Breaking Down Barriers to Care: Behavioral Health Goes Digital
Anxiety affects nearly 30% of people at some point in their lives and often goes hand in hand with depression, which affects about 16 million American adults a year. To add insult to injury, studies show that 4 in 10 U.S. adults who needed mental health treatment in the last 12 months did not get it.
As these numbers continue to climb, accompanied by a flood of demand for mental health care, access to virtual behavioral health care resources may help to address unmet patient need.
Why are so many people with anxiety and depression going untreated?
The reasons are complex and numerous, but stigma, cost, convenience and access to affordable resources are among some of the factors impacting Americans’ ability to get help for their concerns or illnesses. Furthermore, people are often unsure as to whether their feelings require treatment or if it’s situational and something that can be managed through other means, such as changes in lifestyle.
Are the answers in the Cloud?
Virtual care, also referred to as telehealth, may be part of the solution. These resources have steadily gained popularity over the last few years and continue to accelerate —with technological advancement attempting to meet demand. According to the FAIR Health monthly telehealth tracker, telehealth accounted for 5.5% of medical claims in the U.S. in December 2022, and mental health conditions accounted for 62.5% of diagnoses—the top overall diagnosis.
Virtual resources range from video chatting with your primary care physician to texting with a bot for your prescriptions or supplementing mental health care through easily downloadable apps. Virtual care has clear benefits—it’s designed to be convenient, affordable and allows users to get care where and when needed.
Not every situation calls for telehealth and digital solutions are still being studied for how they may fit into overall care planning for individuals, but virtual behavioral health services may play a role in helping to alleviate the mental health crisis.
Consider these three quick tips for evaluating what works best for you:
Tip #1: Establish Your Preferences. Take inventory of what may be of interest for you in terms of care. Not sure? That’s ok. Start with asking yourself the following questions.
- Do you wish to be assessed by a licensed professional for your mental health?
- Would you prefer in-person or virtual care?
- Do you have preferred therapy approaches?
- Can the mental health professional prescribe medication, or do they collaborate with a psychiatrist who will see you if deemed appropriate?
- Do you seek focused problem solving like personalized coaching, rather than treatment?
Tip #2: Speak with Your Primary Care Physician
When considering seeking help, your primary care physician (PCP) can be a great ally and guide—even if you want to explore virtual mental health options. Discuss with your PCP your pre-established goals so they can help point you in the right direction, but it’s also okay if you don’t know exactly what you need. Increasingly, PCPs are interconnected with virtual providers, giving you a holistic approach to your care. Collaboration between primary care teams and mental health specialists has great value, and there is good evidence that your whole-body benefits from mental well-being.
Tip #3: Speak with Your Insurance Provider
When speaking with a customer advocate, describe the care you’d like to receive and ask about available options. They can explain the services that are reimbursed and offer a list of therapists that are covered in-network, helping you understand your choices and keep costs down. They may also help you learn more about the role UnitedHealthcare’s Virtual Behavioral Coaching program might play for you.
Don’t wait to seek mental or behavioral support for yourself or those around you – resources are available.










 Deering Estate
Deering Estate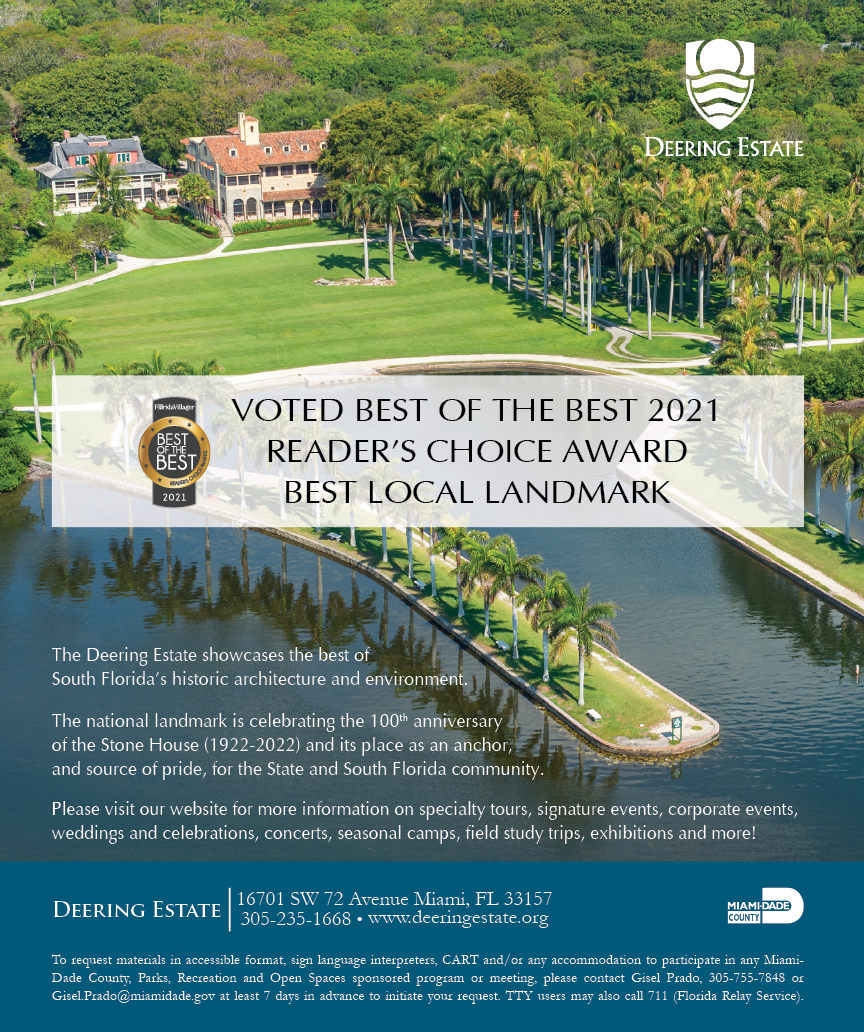
 Massage Envy South Miami
Massage Envy South Miami
 Calla Blow Dry
Calla Blow Dry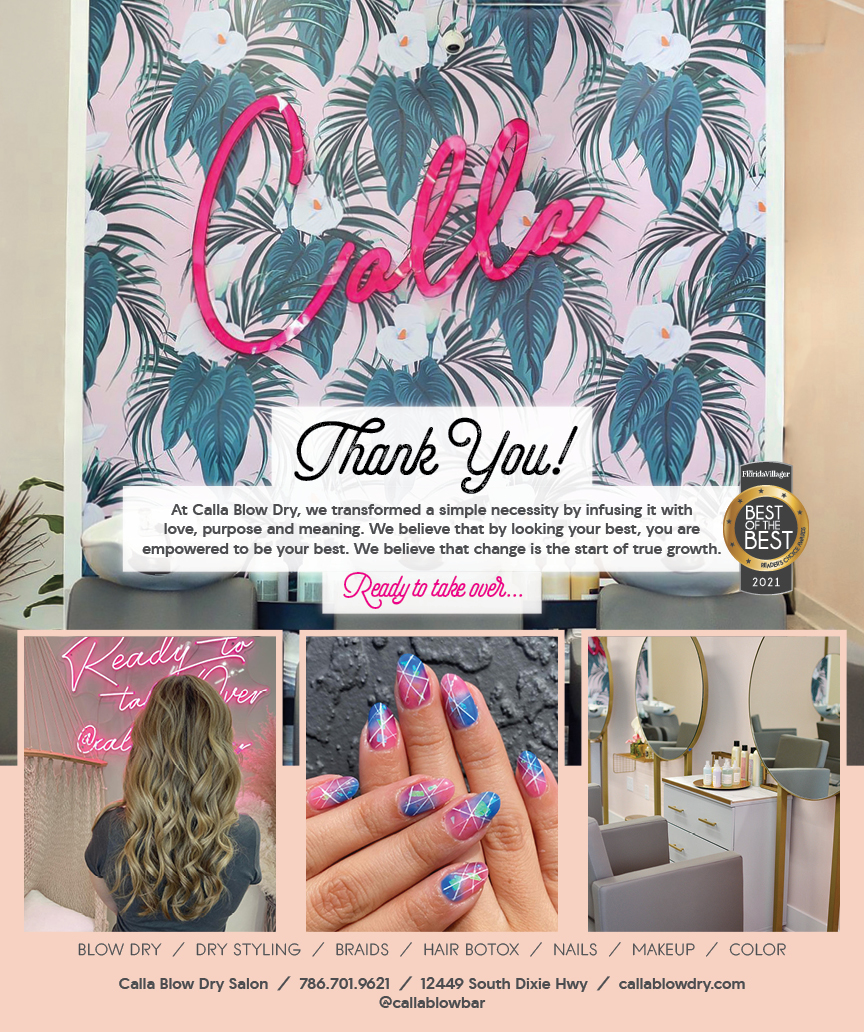
 My Derma Clinic
My Derma Clinic
 Sushi Maki
Sushi Maki
 Sports Grill
Sports Grill
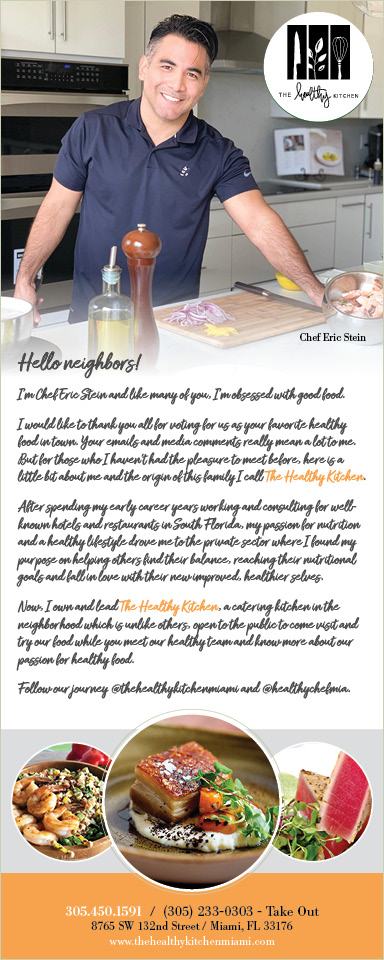
 The Healthy Kitchen
The Healthy Kitchen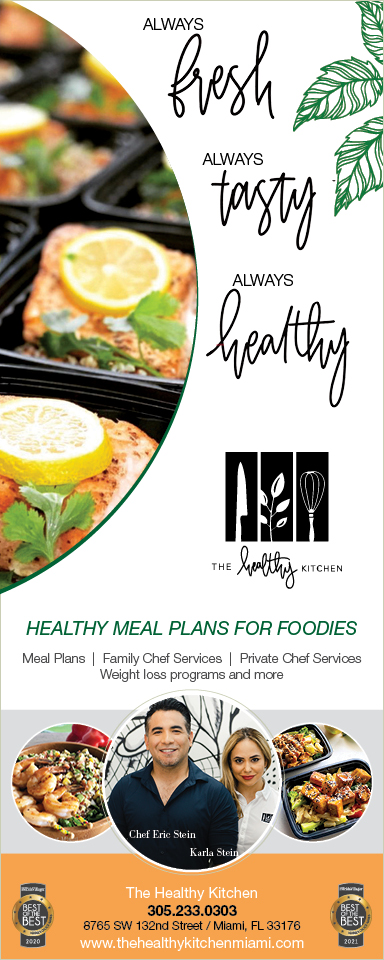
 Golden Rule Seafood
Golden Rule Seafood
 Malanga Cuban Café
Malanga Cuban Café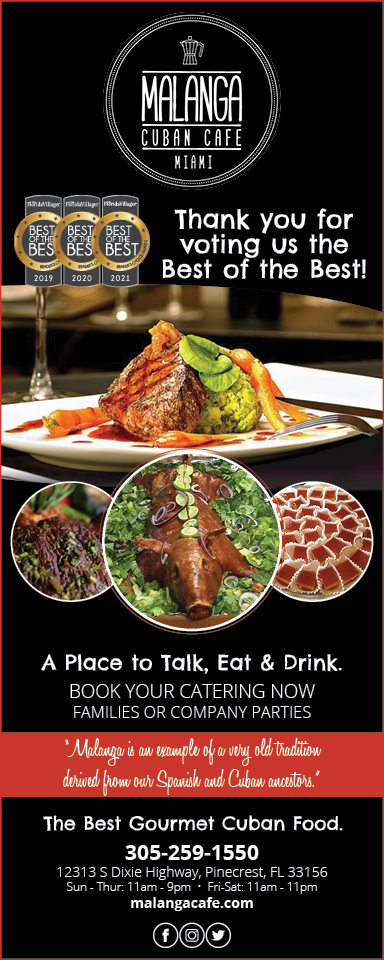

 Kathleen Ballard
Kathleen Ballard
 Panter, Panter & Sampedro
Panter, Panter & Sampedro
 Vintage Liquors
Vintage Liquors
 The Dog from Ipanema
The Dog from Ipanema
 Rubinstein Family Chiropractic
Rubinstein Family Chiropractic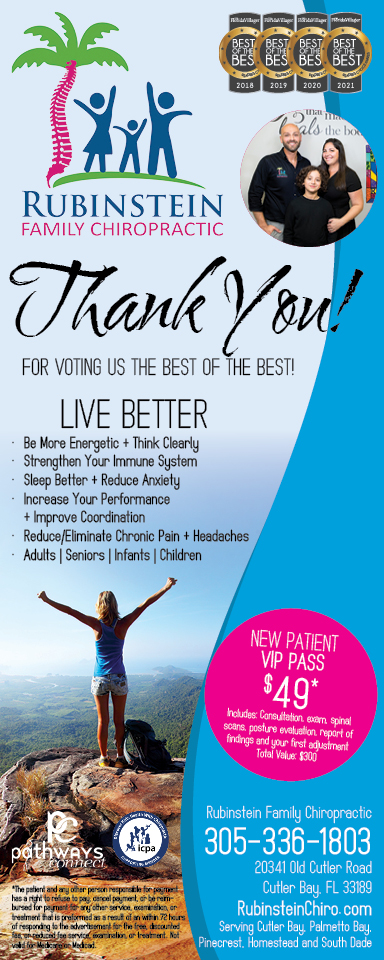
 Your Pet’s Best
Your Pet’s Best
 Indigo Republic
Indigo Republic



 ATR Luxury Homes
ATR Luxury Homes


 2112 Design Studio
2112 Design Studio
 Hamilton Fox & Company
Hamilton Fox & Company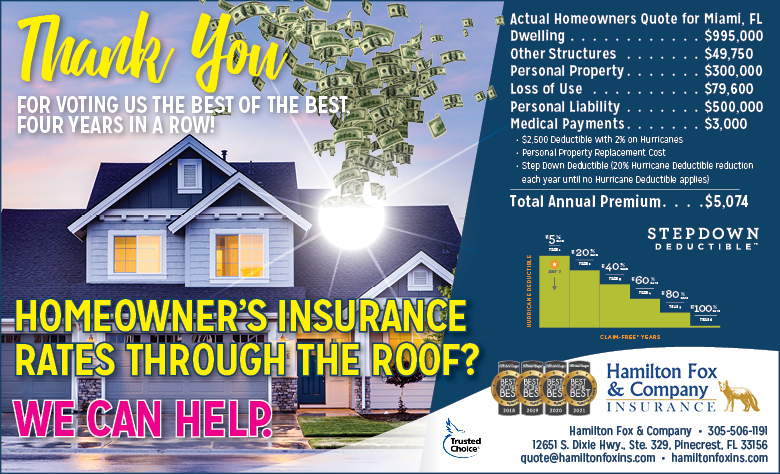
 Creative Design Services
Creative Design Services
 Best Pest Professionals
Best Pest Professionals
 HD Tree Services
HD Tree Services
 Trinity Air Conditioning Company
Trinity Air Conditioning Company
 Cisca Construction & Development
Cisca Construction & Development
 Mosquito Joe
Mosquito Joe
 Cutler Bay Solar Solutions
Cutler Bay Solar Solutions


 Miami Royal Ballet & Dance
Miami Royal Ballet & Dance
 Christopher Columbus
Christopher Columbus
 Pineview Preschools
Pineview Preschools
 Westminster
Westminster
 Carrollton
Carrollton
 Lil’ Jungle
Lil’ Jungle
 Frost Science Museum
Frost Science Museum
 Palmer Trinity School
Palmer Trinity School
 South Florida Music
South Florida Music
 Pinecrest Orthodontics
Pinecrest Orthodontics
 Dr. Bob Pediatric Dentist
Dr. Bob Pediatric Dentist
 d.pediatrics
d.pediatrics
 South Miami Women’s Health
South Miami Women’s Health
 The Spot Barbershop
The Spot Barbershop
 My Derma Clinic
My Derma Clinic


 Miami Dance Project
Miami Dance Project

 Rubinstein Family Chiropractic
Rubinstein Family Chiropractic
 Indigo Republic
Indigo Republic

 Safes Universe
Safes Universe
 Vintage Liquors
Vintage Liquors
 Evenings Delight
Evenings Delight




 Atchana’s Homegrown Thai
Atchana’s Homegrown Thai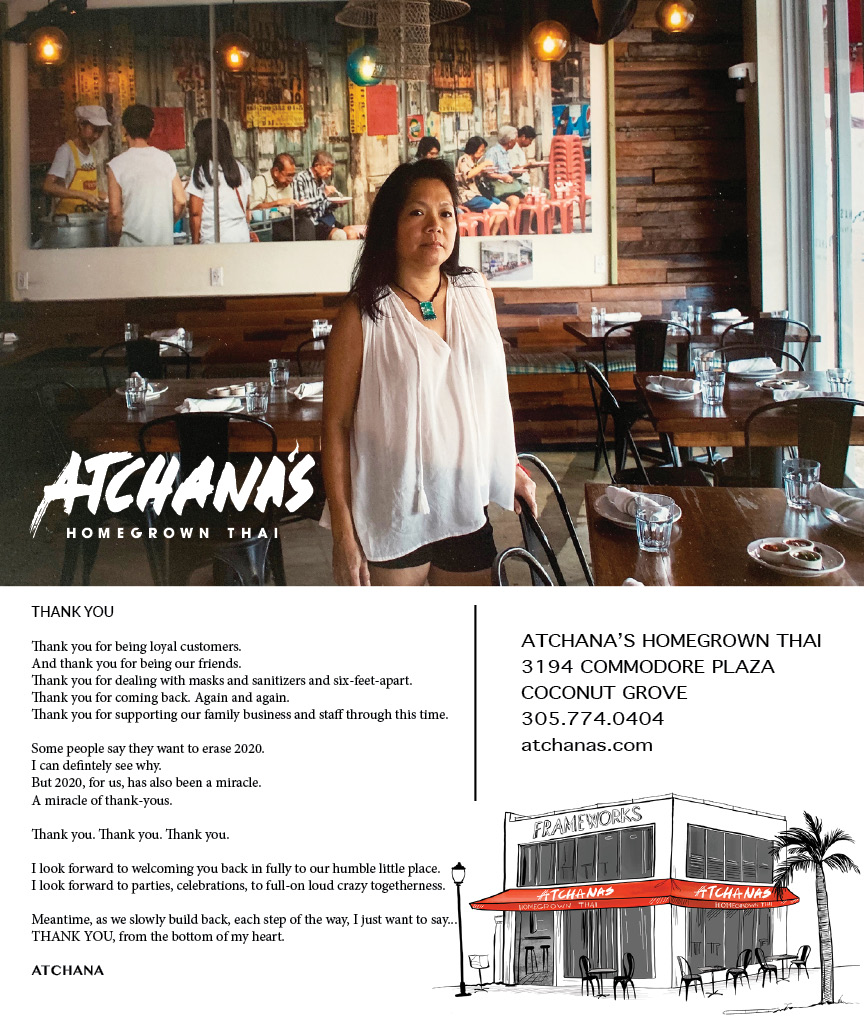
 Baptist Health South Florida
Baptist Health South Florida
 Laser Eye Center of Miami
Laser Eye Center of Miami
 Visiting Angels
Visiting Angels
 OpusCare of South Florida
OpusCare of South Florida
 Your Pet’s Best
Your Pet’s Best




 HD Tree Services
HD Tree Services
 Hamilton Fox & Company
Hamilton Fox & Company


 Creative Design Services
Creative Design Services